There are over 600 species of venomous snakes around the world, and there is a lot of variation in the toxicity or venom between species, and even between snakes of the same species. Venoms are a complex mixture of proteins and peptides that act as enzymes that damage tissues and blood, interfere with blood clotting, and act as neurotoxins to immobilize and kill prey. (The evolution of and variation in venom is an interesting topic on it's own.) The primary purpose of venom is to immobilize, kill, and help digest relatively small prey such as small mammals, fish, amphibians and other reptiles. The toxic effects are painful and debilitating enough to larger animals that the venom also creates a good defense. Many venomous snakes have some type of warning display (distinctive colors, rattles, hoods, etc) to warn and deter predators or other large animals that might stumble upon the snake. Unfortunately, many snakes such as most pit vipers are often well camouflaged and do not always rattle or otherwise warn of their presence. Because of this, even dogs that are "snake trained" can still accidentally step on a quiet snake and be bitten. Snake training for hunting dogs and dogs that live or enter snake habitat may be useful when done by experienced trainers, but is no guarantee that the dog will never be bitten.
Several aspects of snakebite have the potential to make various first aid measures look more effective than they may be. The fact that the patient survives or recovers quickly is not evidence that many first aid measures are effective. While all venomous snakebites have the potential to be deadly, most victims in North America survive (some species such as most elaphids like many Australian snakes, cobras, and coral snakes have more neurotoxic venoms than most vipers such as rattlesnakes, which tend to have more cytotoxic venoms this can affect the mortality rate for snakebite drastically in different parts of the world). Most of the deaths from snakebite in the United States relate to delays in seeking or receiving treatment. There are several reasons many snakebites are not as deadly as they are often perceived to be. The first is that many snakes inject little or no venom when they bite. Snakes "want" to escape and save their venom for catching and consuming prey, and if a warning dry bite will allow them to escape, then that is what they will do. A second reason is that there is quite a bit of variation in the toxicity of venom between different species of snakes and even between individuals of the same species because of age, size, and other factors. Also, some non-venomous or mildly venomous snakes mimic venomous species and will bite, but do not have very toxic venom or any venom at all. This means that some snake bites may be misidentified as venomous when they are not. It is often not advisable to attempt to catch or kill a suspected venomous snake as this can result in another bite. Because of misidentified bites, and bites that are from venomous snakes, but the snake releases very little or no venom, a significant number of snakebites are not as serious as they might first appear, and these bites can make first aid measure look more effective than they are.
Medical treatment;
The primary medical treatment for envenomation is treatment with antivenom (also spelled antivenin) and supportive care to treat the shock and complications caused by the venom and sometimes allergic reactions to the antivenom. Antivenom is produced by injecting small amounts of venom intravenously into an animal (usually horses, or sheep). over time and many injections, the animal develops antibodies to the proteins and peptides that make up the toxins in venom. Serum is collected and the antibodies are freeze dried for use as antivenom. Antibodies to the venom from a specific species are the most effective for treating bites from that species, but often antivenom is made using venom from several species. This is called polyvalent antivenom. In North America antivenom is usually polyvalent crotalidae antivenom, which is made with venom from several species of rattlesnake from north and central america and is effective for treating any species of rattlesnake bite. There is some variation in venom, and snakes such as the Mohave rattlesnake have more neurotoxic venom than most other rattlesnakes, and may not respond as well to polyvalent antivenom as well as bites from some other species. Crofab antivenom approved by the FDA in 2001 is made using mojave rattlesnake venom and is more effective against mojave venom than older antivenoms. Crofab is very expensive and is rarely used by veterinarians. The situation is different in different parts of the world. In Australia, a test is available to confirm if venom is present and what type of venom. This allows the use of antivenom specific to the bite, and conserves the more expensive polyvalent antivenom.
Other treatments such as intravenous fluid therapy may be used to help keep patients hydrated and to treat shock and fluid loss associated with the bite. Antibiotics may be used to treat secondary infections which may be common in bites from rattlesnakes which damage tissues. These treatments do not directly affect the venom the way antivenom does, however. Since antivenom contains animal proteins, it can cause acute or delayed allergic reactions which are treated with antihitamines and steroids. Again, these drugs are useful for complications from the antivenom, but do not affect or treat the venom itself. Some veterinarians treat snakebites with fluids, antibiotics and steroids when antivenom is not available or when it is beyond the owner's means, but the steroid portion of the treatment is probably not effective and may even be harmful in some cases. This may also be kept as part of the treatment protocol because steroids are often given to prevent reactions to the antivenom, and veterinarians who do not treat snakebite often may remember the use of steroids without remembering why they are used (for reactions to antivenom) in the heat of the moment.
Rattlesnake vaccine
There is a rattlesnake vaccine available in the United States that is provisionally licensed for use in dogs by the FDA. This is neither a treatment nor a first aid method, but is designed to stimulate antibody production to snake venom-in effect creating "anitvenom" in the dog's bloodstream prior to any bite. This vaccine has been demonstrated to produce antibodies capable of neutralizing venom in laboratory tests, but has not been tested in deliberate "challenge" trials, and probably will not be. The vaccine is produced using western diamondback venom, and provides variable effectiveness against other species. High doses of venom can still overwhelm the antibodies produced, so the vaccine is no guarantee of survival. The company claims that the antibodies produced in an average sized dog are the equivalent to 2-3 vials of antivenom, which is often enough to treat many bites. Due to the expense and sometimes limited availability of antivenom for veterinary use, this vaccine might be worth using if your dog is at high risk for rattlesnake bite. Dog that live in rattlesnake habitat or who hike or hunt in areas with rattlesnakes might be dogs that would benefit. It is certainly not necessary for dogs that never leave town and are not likely to encounter snakes. I have heard some rumors of some veterinarians charging hundreds of dollars for this vaccine-the vaccine is fairly inexpensive and should not be much more expensive than any other veterinary vaccines.
First Aid-what may work and what does not.
Tourniquet/pressure bandage;
One of the oldest first aid measures for snakebite is the use of a tourniquet to keep the venom from spreading from the site of the bite. This is not recommended for several reasons. If the tourniquet is left in place too long, the loss of blood supply can damage or kill the limb even in the absence of venom. In the case of bites from snakes such as rattlesnakes and other vipers with cytotoxic venom that damages tissue, a tourniquet can increase the damage caused by the venom, while adding damage from loss of circulation. In the case of snakes with neurotoxic venom such as elaphids (most australian snakes, cobras, coral snakes, and a few others) an immobilizing pressure bandage may be useful. If you are not sure about the type of bite, it is probably better not to use this type of bandage, especially in the North or South America, where rattlesnake bites are much more common than coral snake bites.
Suction;
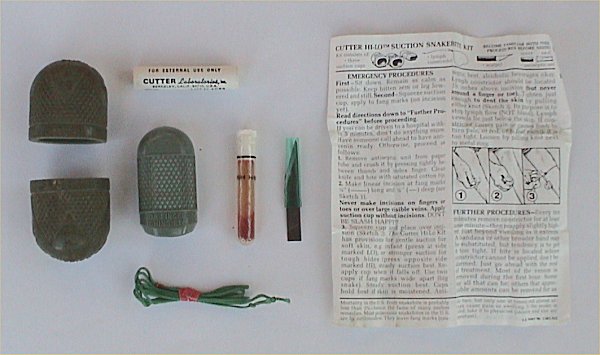
picture from wikipedia snakebite page.
Another old first aid treatment is suction of the bite. Older snakebite kits such as the Cutter kit pictured above (I had one of these when I was a kid-fortunately I never had an opportunity to use it.) often contained a scalpel blade and a string tourniquet. Making incisions increases the chance of infection and runs the risk of serious bleeding from cut blood vessels, or nerve damage, and does not really help remove venom. The tourniquet has the problems discussed above. These older kits also came with the rubber suction cups pictured that did not really provide very effective suction. A newer version of this type of kit is the Sawyer Extractor. This kit has the advantage of providing much stronger suction and does not contain a scalpel blade or a tourniquet. However, it is still not very effective in bites where the venom is deeply injected below the skin surface and may cause more localized tissue necrosis. It may be difficult to use on animals due to their furred skin interfering with the suction seal. This kit is fairly cheap ($15 U.S.) and may be useful for minor injuries like bee stings, but don't count on it to remove significant amounts of venom. If you do use it, apply it within the first minute or two of the bite and don't leave it in place for more than a few minutes at a time. Also don't waste time fiddling with it if it will delay getting to the vet or hospital.Electric shock;
One first aid method that was briefly popular in the 1980's was electric shock to the area of the bite. This usually involved shocking the area of the bite with various devices ranging from 12 volt automotive batteries to stun guns. Probably because of mild bites, there are anecdotal reports of effectiveness, but this method can result in electrical burns and damage to tissues, and does not seem to have any effect when tested under controlled conditions.
Vitamin C;
Another old treatment that has been around for a long time is the injection of large doses of vitamin C. This seems to date back to the 1930's soon after the chemical structure of vitamin C was worked out, and it was being promoted as a cure for anything from tuberculosis to cancer. It is still a popular remedy and can be found on many veterinary homeopathic naturopathic and other alternative medicine(quackery) sites. It also seems to be popular in Australia for some reason, possibly due to many farmers and pet owners living some distance from veterinary services and desiring an inexpensive and quick remedy to give. Various sites recommend giving large doses of vitamin C orally, intravenously, or intramuscularly. There is no real reason that large doses of Vitamin C should counteract snake venom, and this interesting site shows a series of cases in a goat herd, where the farmer carefully recorded the effects or lack thereof, of vitamin C injections in animals suspected of being bitten. Interestingly, several cases that survived turned out to be from non-venomous snakes, or "dry" or mild bites from venomous snakes or problems unrelated to snakebite. The animals confirmed to have serious snakebite died despite vitamin C injection. Vitamin C is acidic and is very painful when injected intramuscularly, and in at least one of the goats reported above, apparently caused sterile abscesses to form after the injections. Again, this treatment is not really any better than placebo, and may be harmful in some circumstances.
In conclusion, most first aid treatments for venomous bites are ineffective or minimally effective, and sometimes can cause injury themselves. Don't spend too much time trying to apply first aid to a victim of venomous snakebite. The best chance for humans or animals in such circumstances is getting to professional medical care as quickly as possible. As a friend of mine who is an expert in primitive desert survival techniques and wilderness first aid says, "the best first aid for snakebite is your car keys". Getting to a medical provider who can evaluate the severity of the bite and administer antivenom if necessary is the best thing to do in this unfortunate situation. Time spent trying to apply ineffective first aid, or even worse, self treating with vitamins or some other "natural" remedy can make the difference between surviving the bite and dying from it, and not in a positive way. Snake venom is natural too, and is one of the most toxic substances found anywhere.






I have sucessfully treated a 5 month old Scottish Deerhound with a serious rattle snake bite to the face,Pacific Coast Diamondback, which swelled his head up like a football to where he could not drink or eat with 2kmils of oral vit.C every 2 hrs,and drizzeled water in his mouth with a sports bottle on a Monday.In 24hrs the swelling was nearly gone and he was back to eating and drinking.I continued the 2kmils every 4hrs after that for another 24hrs and he continued a speedy recovery.I continued to dose every 6 hours then 8 and so on,by Friday he was completely well with barely a scab,absolutely no necrotic tissue...So I would say your statements on Vit.C to be political, bias,and he said she said,they say.For us it was a safe and sucessful option,as we have gone the other route with a vet,antivenom,antibiotics,with more neg.side effects,and $2,500
ReplyDelete@animallover; nice anecdote-if you had read the post you would understand why it is basically worthless as evidence. There is great variability in snakebites and that was probably the normal course for that particular bite in a large dog. I am glad he did well, but there is really no evidence that the Vit. C did anything. It is not unusual to provide supportive care when the antivenin is unavailable or unaffordable, with often similar results. Again, I am happy that your dog did well, but it does not prove that the Vit. C did anything other than give you something to do.
ReplyDeleteMy dog was bitten by a snake of some source thinking maybe a rattle snake in the leg. Took her an hour away t the vet hospital the leg was swollen she was in shock. We told the vet on staff that night what we thought might have happened and they treated her with antibotics, and pain meds, and fluids then 9 hours later said she has taken a turn for the worst and ask to immediately give her the anti venom but did not to begin with b/c of a cost issue we told them anything we will pay but give us till the morning the next day after many hours my poor dog died I was told it was not b/c of the time lapse it was b/c she did not respond. We are heart broken and can not get past this can anyone here tell me anything to help us sincerely BigBucfan@Hotmail.com thank you kindly Deb
ReplyDeleteHey Deb, We just lost our 10 1/2 year old Corgi from something totally unrelated to a snake bite. However, I was looking up snake bites because our friends Jack russell terrier was bitten today and I came upon your message and it just broke my heart. I am SO sorry you lost your dog. We love our pets so much and we treat them like little children. I still cry on and off during the day because I miss my little Winston so much. It is so hard to look around and not see him. He followed me every where, was by my side constantly, slept in our room, etc. He died 11 days ago and I don't know how long it will be before my husband and my son and I are not feeling so devasted and sad. If you want to share anything or just need a friend to email who knows how you feel, email me: Joyce jrandall1258@yahoo.com I'm from Port St. John, Florida, but we own and operate a campground in Pikeville, TN and that's where we are now. I just wanted you to know that someone knows how you feel and I'm so sorry.
DeleteSorry to hear about your dog, Debora. Every case is different, and it is difficult to comment based on limited information, but it does sound like your dog suffered a venomous bite. Antivenin does work better when given early when there are signs (swelling, shock, etc) of serious envenomation. In some cases it can take quite a bit of antivenin, one or two vials may not have been enough in your particular case. Very sorry for the loss of your dog.
ReplyDeleteDebora -- you never know with rattlesnake bites. So much depends on how big the dog is, how big the snake is, whether it injected a little venom or a lot, whether the bite struck a big muscle (bad) or skin over bone (better), and just how the dog responds. If your poor pup had bad luck in one or more of these ways, it's just the way things happen sometimes.
ReplyDeleteBut there is a rattlesnake vaccine for dogs. It's not expensive and it works really, really well. All our dogs get it now, since we had a terrible experience with a dog shortly after we moved out here. It turns what can be a horrible medical problem (or even death) into something that the dog can survive easily with just some antibiotics, steroids, and pain medication.
Glucocorticoids, nonsteroidal antiinflammatory drugs (NSAIDs) and antihistamines are not included in the majority of recommended treatment protocols by world authorities; however, there are some reports that describe their use. Currently, only the use of Antivenin improves clinical outcome, pain and swelling. Antimicrobial therapy and blood products are used only when clinically indicated.
ReplyDelete